


Diabetes is a chronic metabolic condition marked by high blood glucose levels. Type 2 diabetes — the most common form — typically affects adults and occurs when the body becomes insulin-resistant or doesn’t produce enough insulin. Type 1 diabetes, on the other hand, is when the pancreas produces little to no insulin.
India is often referred to as the diabetes capital of the world, with around 60 million people affected. The condition significantly increases the risk of heart attacks, strokes, kidney failure, nerve damage, vision loss, and limb amputation.
While type 2 diabetes can’t be fully prevented, early diagnosis is key to managing it effectively. Cost-effective interventions — including blood glucose control through diet, physical activity, medication if needed, blood pressure and lipid management, and regular screening for eye, kidney, and foot complications — can greatly improve outcomes.

Chronic respiratory diseases (CRDs) such as asthma, chronic obstructive pulmonary disease (COPD), and bronchiectasis affect millions globally and are a leading cause of morbidity and mortality. These long-term conditions limit airflow in the lungs, often resulting in breathlessness, persistent cough, wheezing, and reduced physical activity.
CRDs are primarily caused by environmental exposures like tobacco smoke, air pollution, occupational hazards, and genetic factors. While they are not fully curable, early diagnosis, appropriate treatment, and lifestyle modifications can help manage symptoms effectively and prevent disease progression.
At Mankind Specialities, we recognize the burden of CRDs and are committed to supporting better respiratory outcomes through evidence-based therapies and innovative inhalation solutions. Our goal is to enable patients to lead fuller, more active lives by improving lung function, reducing exacerbations, and enhancing overall quality of life.

Cardiovascular disease is the leading cause of non-communicable disease (NCD) deaths in India, accounting for 1 in 4 fatalities. Many heart attacks can be prevented through early detection and treatment in high-risk individuals. A regimen including aspirin, statins, and blood pressure medications can reduce deaths in those aged 40–79.
CVD includes:
Key risk factors: tobacco use, unhealthy diet, physical inactivity, obesity, high blood pressure, diabetes, and high cholesterol. Treatment may involve surgery (e.g., bypass, angioplasty), heart transplants, and medical devices like pacemakers or artificial valves.

Hypertension, or high blood pressure, affects 29.8% of Indians and caused 1.6 million deaths in 2016. Often symptomless, it is known as the “silent killer.”
Risk factors include:
In severe cases, symptoms may include headaches, vision changes, irregular heartbeat, chest pain, and fatigue. Regular monitoring is essential. Prevention involves reducing salt intake, improving diet, increasing physical activity, and avoiding tobacco and alcohol


Dyslipidemia refers to abnormal blood lipid levels — including high LDL (bad cholesterol), low HDL (good cholesterol), and high triglycerides.
Though often without symptoms, it increases the risk of coronary artery disease (CAD) and peripheral artery disease (PAD), which can lead to heart attack and stroke. It’s usually detected through routine blood tests.
Severe or untreated cases may show signs like chest pain, leg pain, fatigue, shortness of breath, swelling, or heart palpitations. Managing lipid levels is crucial to reducing cardiovascular risk.

Cancer is a condition where abnormal body cells start growing uncontrollably and may extend to other organs or tissues. While normal cells, with the checks of the body, do not grow and destroy adjacent tissues, cancer cells escape the control of the body and continue to grow and invade nearby tissues, sometimes resulting in tumors or influencing blood and immune cells. Cancer is an emerging health problem in India. In 2022, an estimated 1.46 million new cases were registered, with a projected increase to 1.57 million by 2025. The likelihood of getting cancer during one’s lifetime is one out of nine Indians. The prevalent cancers are lung men and breast in women.


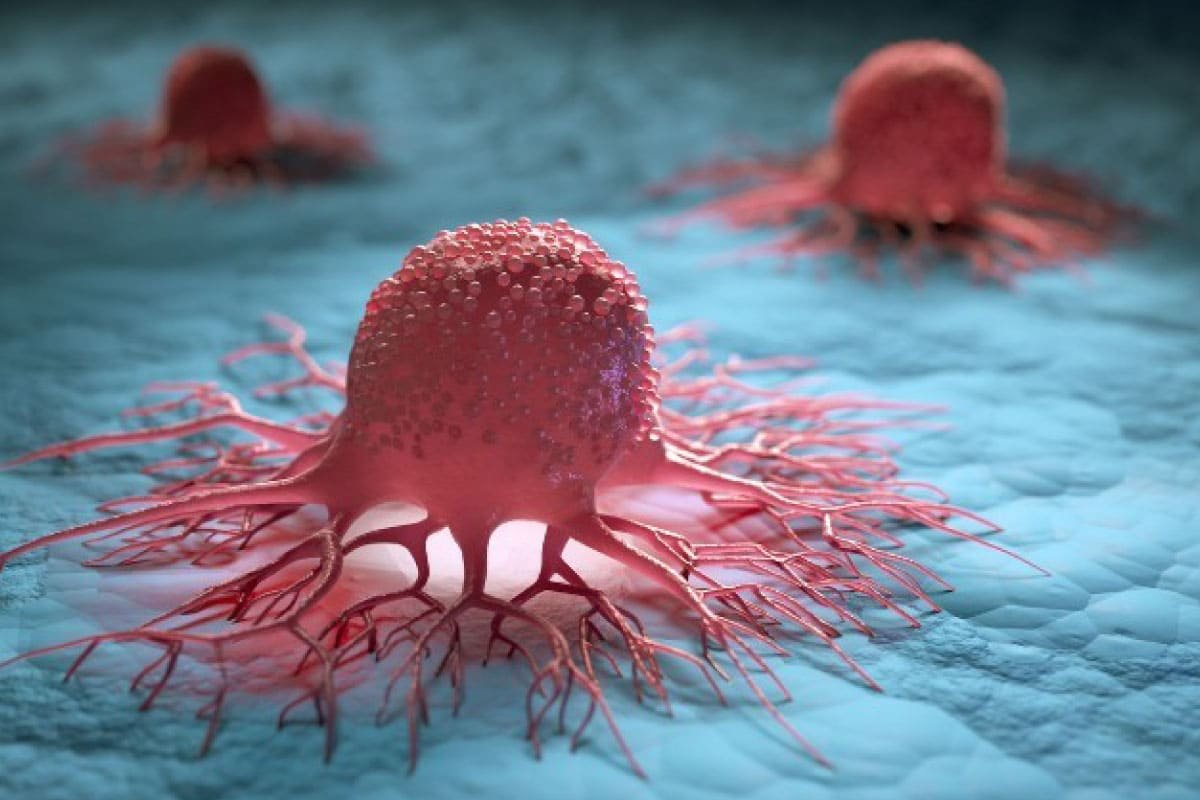
Solid tumors are abnormal tissue masses that usually don’t have liquid areas or cysts. They could be malignant (cancerous) or benign (non-cancerous). About 90% of adult cancers are solid tumor cancers, which can arise in a variety of organs, such as the kidney, prostate, lung, breast, and colon. These cancers are categorized according to the kind of cell or organ they start in, including:
Carcinomas: Develop in the organ lining, such as the colon, lung, or breast.
Sarcomas: Start in supporting or connective tissues, such as muscle, fat, or bone.
Lymphomas: Rather than appearing as blood cancers, lymphomas are solid masses that affect
lymphatic tissues.
Solid tumors develop into a mass that may infiltrate adjacent tissues and occasionally spread through the blood or lymphatic system to other parts of the body. Many solid tumor cancers now have better management and results thanks to early detection and advancements in targeted therapies.

Hematological (blood) cancers develop in immune system cells or in tissues that form blood, like bone marrow. These cancers usually affect blood, bone marrow, and lymphatic tissues rather than forming a distinct mass like solid tumors do. Common types are:
Leukemia: Causes an excess of aberrant white blood cells and begins in the bone marrow.
Lymphomas: White blood cells called lymphocytes are the source of lymphoma, which typically affects lymph nodes and other lymphatic tissues.
Multiple Myeloma: Another type of immune cell produced in the bone marrow, plasma cells, are the starting point for multiple myeloma.
Hematological cancers impair immunity and the body’s capacity to fight infections by interfering with the normal production and function of blood cells. Chemotherapy, immunotherapy, targeted therapy, or stem cell transplantation are commonly used forms of treatment.



India has over 4 million people living with Alzheimer’s, the third-highest burden globally. Yet, it’s often underdiagnosed, as many view memory loss as a normal part of ageing rather than a sign of a neurodegenerative disease.
Alzheimer’s leads to the destruction of brain cells and impairs memory, thinking, and communication. As it progresses, cognitive abilities decline severely. Risk factors include genetics, ageing, tobacco and substance use, poor diet, inactivity, pollution, and head injuries. While there is no cure, cholinesterase inhibitors can help slow Alzheimer’s progression. Emotional support and therapy also play a key role in management.
Healthy lifestyle choices — a nutritious diet, physical activity, and avoiding tobacco — may reduce the risk of neurological conditions.

A stroke occurs when blood supply to part of the brain is interrupted, causing loss of function in the body.
Stroke is a leading cause of death and disability in India, with rising cases. In 2017, global stroke prevalence reached 104.2 million.
FAST is the global protocol for early identification:
Clot-busting drugs are effective only within a 3–4.5 hour window from symptom onset. Prevention includes quitting smoking, managing blood pressure, maintaining a healthy weight, regular exercise, and a balanced diet.


Gastroenterological disorders involve conditions affecting the gastrointestinal (GI) tract, from the mouth to the anus.
Constipation involves infrequent, difficult, or incomplete bowel movements with hard, dry stools. It can be primary (functional) or secondary (due to lifestyle, illness, or medication).
🔸 Common symptoms include:
Complications: Hemorrhoids, anal fissures, rectal prolapse, and fecal impaction.

Types:
Causes:
Symptoms:
Complications:
Diagnosis:
Treatment:
Prevention Tips:
Hemorrhoids are swollen veins in the lower rectum or anus, common in all age groups. They are classified as internal, external, or mixed.
🔸 Causes: Chronic constipation/diarrhea, straining, pregnancy, heavy lifting, and genetics.
Symptoms:
Diagnosis: Clinical exam, digital rectal exam, and procedures like anoscopy or colonoscopy.
Complications: Thrombosis, fissures, strangulation, anemia.


Urinary Health
Urinary health plays a key role in overall well-being, yet issues like urgency, leakage, or infections are often overlooked due to stigma. At Mankind, we aim to raise awareness, encourage early diagnosis, and support lifelong urological wellness—for both men and women.
Common Urinary Conditions
BPH (Benign Prostatic Hyperplasia)
Non-cancerous prostate enlargement, common after 40. Symptoms: weak stream, frequent urination (especially at night), difficulty starting, and incomplete emptying. Treated with medications, lifestyle changes, or minor procedures.
OAB (Overactive Bladder)
Causes sudden, frequent urges (over 8 times/day) and leakage. Managed with behavioral therapy, medications, and pelvic floor exercises.
UTI (Urinary Tract Infection)
Bacterial infection of the bladder, urethra, or kidneys. Symptoms: burning while urinating, pelvic pain, cloudy or smelly urine, and frequent urges. Common in women; treated with antibiotics and fluids.
Mankind is a transnational pharmaceutical company that started operations in 1995. Committed to a healthier & happier world, Mankind Pharma strives to provide accessible & affordable healthcare whilst achieving best quality industry standards.
Mankind has grown exponentially to become India’s No.1 company as per Prescriptions.
Mankind Specialities is a super specialty division of Mankind Pharma, which started operations in Mumbai in the financial year 20-21 with the vision of serving the lives of millions of patients with innovative solutions, by offering quality and affordable products.
Powered by Trendingg © 2025 Mankind Specialities. All Rights Reserved.
CIN No: U74899DL1991PLC044843
Gastroenterology is a medical specialty focused on the study, diagnosis, and treatment of disorders affecting the digestive system, which includes the esophagus, stomach, small intestine, colon and rectum, pancreas, gallbladder, bile ducts, and liver.
Gastrointestinal conditions such as constipation and hemorrhoids can cause distressing symptoms, whereas chronic gastrointestinal diseases such as inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), peptic ulcer disease, and chronic liver disease can affect millions of people worldwide and cause significant morbidity and mortality. These long-term conditions disrupt normal digestive function, frequently resulting in symptoms such as abdominal pain, bloating, diarrhea or constipation, blood in the stool, unintentional weight loss, and nutritional deficiencies. Chronic gastrointestinal diseases are caused by a combination of genetic predispositions, immune system abnormalities, lifestyle factors, infections, and environmental exposures like poor diet, stress, and certain medications. While most chronic gastrointestinal diseases are incurable, early and accurate diagnosis, combined with comprehensive medical management, dietary changes, and regular follow-ups, can help to control symptoms, improve quality of life, and lower the risk of serious complications. Medication and patient education must be administered on time to prevent disease progression and ensure the best long-term results.
Constipation
Constipation is GI condition pertaining to large intestine, characterized by bowel moments that are difficult, infrequent, and often incomplete evacuation, accompanied by the passage of hard, dry stools. It may be classified as either primary (functional), resulting from issues with the normal function of the colon or rectum, or secondary, which is due to factors such as poor diet (low fiber or inadequate fluids), sedentary lifestyle, underlying medical conditions (like hypothyroidism or diabetes), or as a side effect of certain medications (including opioids, antacids, and some antidepressants).
Common symptoms of constipation include:
Complications of unmanaged constipation are:
Recognizing the signs and addressing constipation early, through lifestyle modifications, dietary changes, and, when necessary, medical treatments are important to prevent these complications and maintain healthy bowel function.
Hemorrhoids:
Hemorrhoids, also known as piles, are swollen and inflamed veins located in the lower part of the rectum or around the anus. They are a very common condition affecting people of various age groups, and can be classified into:
Causes
A variety of factors can increase pressure on the veins in the rectal and anal area, leading to hemorrhoids:
Symptoms
Internal hemorrhoids:
External hemorrhoids:
Diagnosis
Complications
If untreated or aggravated, hemorrhoids can lead to several complications:
Management Overview
Treatment depends on severity and presentation:
Early diagnosis and appropriate management usually relieve symptoms and prevent progression or complications. Persistent or severe symptoms should prompt evaluation by a healthcare provider for tailored treatment and to exclude more serious disease.